Responding to 7 pro-choice claims about embryonic hearts

1. Embryos don’t have hearts. They have groups of pulsing cells where the heart will eventually form.
The embryonic period is defined as the first stage of the pregnancy up to 11 weeks gestation. The embryonic heart–including atria, ventricles, and related structures–is present by 6 weeks gestation. We have collected multiple scientific and medical sources explaining as much here.
2. Embryos don’t have heartbeats. They have rudimentary electrical activity of cardiac cells.
By 6-7 weeks gestation, the embryonic heart uses coordinated muscle contractions to unidirectionally pump blood through the embryo’s veins to facilitate exchange of oxygen and carbon dioxide. Here are peer-reviewed publications and textbooks explaining as much.
3. Heart muscle tissue isn’t fully organized until 20 weeks.
Yes, the embryonic heart is not a fully developed adult heart, just as the embryonic lungs, brain, and so forth have more development to undergo. We aren’t arguing that embryos have the physiological development of adult humans. We’re acknowledging that embryos have hearts and heartbeats.
This claim about heart muscle tissue stems from a MedicineNet article discussing research on fetal development. The same article readily acknowledges that embryos have hearts, stating “British researchers analyzed scans of the hearts of healthy fetuses in the womb and found that the heart has four clearly defined chambers in the eighth week of pregnancy” and “Human fetuses have a regular heartbeat beginning at about 22 days of pregnancy.”
4. A heartbeat has no moral significance. Dogs and cats have heartbeats. We can get cardiac cells to pulse or “beat” in a petri dish.
We agree the heartbeat doesn’t make an embryo a person, but personhood isn’t the only relevant factor when considering moral significance. First, the presence of a functioning cardiovascular system so early in the pregnancy (about 6-7 weeks gestation) undermines the “clump of cells” rhetoric that misleads people to think embryos are less developed than is actually the case. Second, the presence of an embryonic heartbeat is one indicator of the pregnancy’s viability, which has great moral significance for countless parents.
[Read testimonials from people who became pro-life in part because of seeing and hearing their prenatal children’s heartbeats.]
5. The presence of a heartbeat doesn’t guarantee live birth.
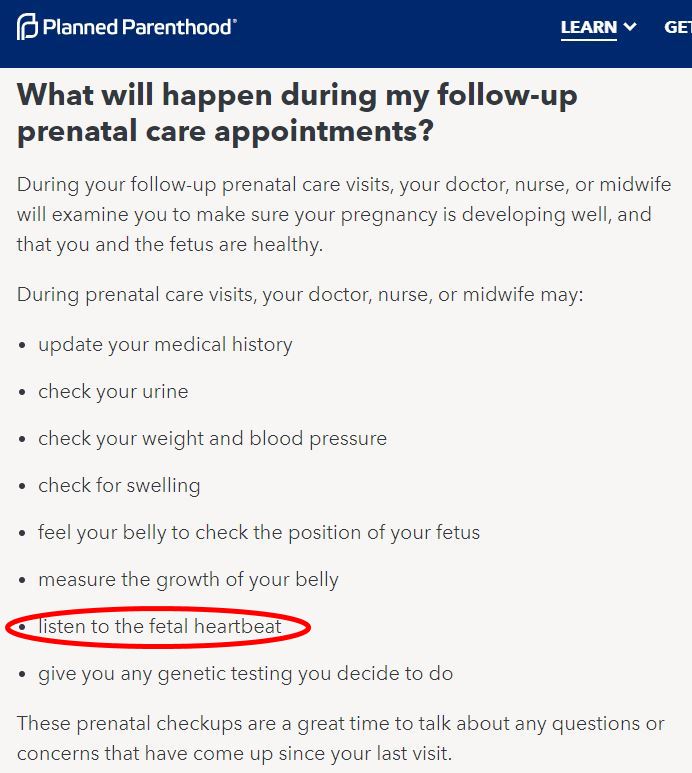
But it does indicate increased likelihood of live birth. Obviously the lack of a heartbeat after 6-7 weeks would mean the embryo has died. Additionally the presence of a heartbeat with the correct rate (beats per minute) is an indicator of the health of the embryo. That’s why it’s standard practice for medical professionals to assess both presence and rate of embryonic heartbeat when providing prenatal care.
6. The presence of a heartbeat has no particular significance in determining the viability of the pregnancy.
That’s inaccurate. An embryonic heart rate that’s too slow is a significant predictor of miscarriage, and one that’s in the right range is an effective predictor of pregnancy continuation. Sources:
- “Prediction of miscarriage in women with viable intrauterine pregnancy — A systematic review and diagnostic accuracy meta-analysis,” Pillai et al., European Journal of Obstetrics & Gynecology, January 2018, 220:122-131: “Among the ultrasound scan markers, fetal bradycardia [a slower than normal heart rate]…showed sensitivity of 68.41%, specificity of 97.84%, positive likelihood ratio of 31.73 (indicating a large effect on increasing the probability of predicting miscarriage).” “A cut-off of < 110 beats per minute (bpm) predicts miscarriage best.”
- “Clinical and Ultrasound Evaluation of Early Threatened Miscarriage to Predict Pregnancy Continuation up to 28 Weeks,” Shaamash et al, Journal of Ultrasound in Medicine, 2020, 39:1777-1785: “After a single US [ultrasound] scan, the presence of at least an E/FHR [embryonic/fetal heart rate] of greater than 113 bpm… appeared as a simple, measurable, and effective predictor of pregnancy continuation up to 28 weeks.”
- “Prediction of pregnancy loss by early first trimester ultrasound characteristics,” DeVilbiss et al, American Journal of Obstetrics & Gynecology, August 2020, 223(2):242.e1-242.e22: “Low fetal heart rate and small crown-rump length…were independent predictors of clinical pregnancy loss.”
7. The sound parents hear during early prenatal visits isn’t actually the heart beating. It’s a sound the ultrasound produces when it translates electrical activity to auditory signal.
The ultrasound isn’t detecting electrical activity; it’s detecting movement. “In brief, M-Mode gives a real-time representation of a moving object.” (Source.) In this case it’s detecting the movement of the heart as it contracts and relaxes in order to pump blood, i.e. the heart’s beat. It translates that rhythmic movement into a rhythmic sound we can listen to. The fact that we can’t hear the heart beating without technological aid is an indicator of how very small the embryonic heart is, not an indicator that it isn’t really beating.
[Read more – Opponents of heartbeat bills don’t understand how ultrasounds work]
If you appreciate our work and would like to help, one of the most effective ways to do so is to become a monthly donor. You can also give a one time donation here or volunteer with us here.




Leave a Reply
Want to join the discussion?Feel free to contribute!