How doctors can build trust with parents of children with Trisomy 13 or 18
I recently read this article in the journal Palliative Medicine: Building trust and improving communication with parents of children with Trisomy 13 and 18. Trisomy 13 and 18 are common life-limiting conditions associated with major disabilities. This article explores the experiences of parents of children with Trisomy 13 or 18, focusing on the parents’ interactions with the medical community and which behaviors from clinicians built trust. This blog post is a brief summary, focused primarily on parents’ own descriptions of their experiences with their medical providers.
What the article studied
This article focused on two questions:
- “Please tell us about the most helpful comments or actions made by healthcare providers” and
- “Please tell us about the most unhelpful or insensitive comments or actions made by healthcare providers.”
Main takeaway:
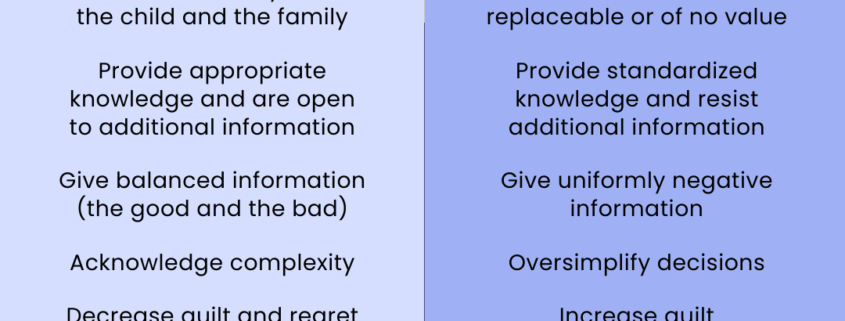
When parents described positive and supportive interaction with clinicians, the overarching theme, present in 88% of open-ended answers, was trust.
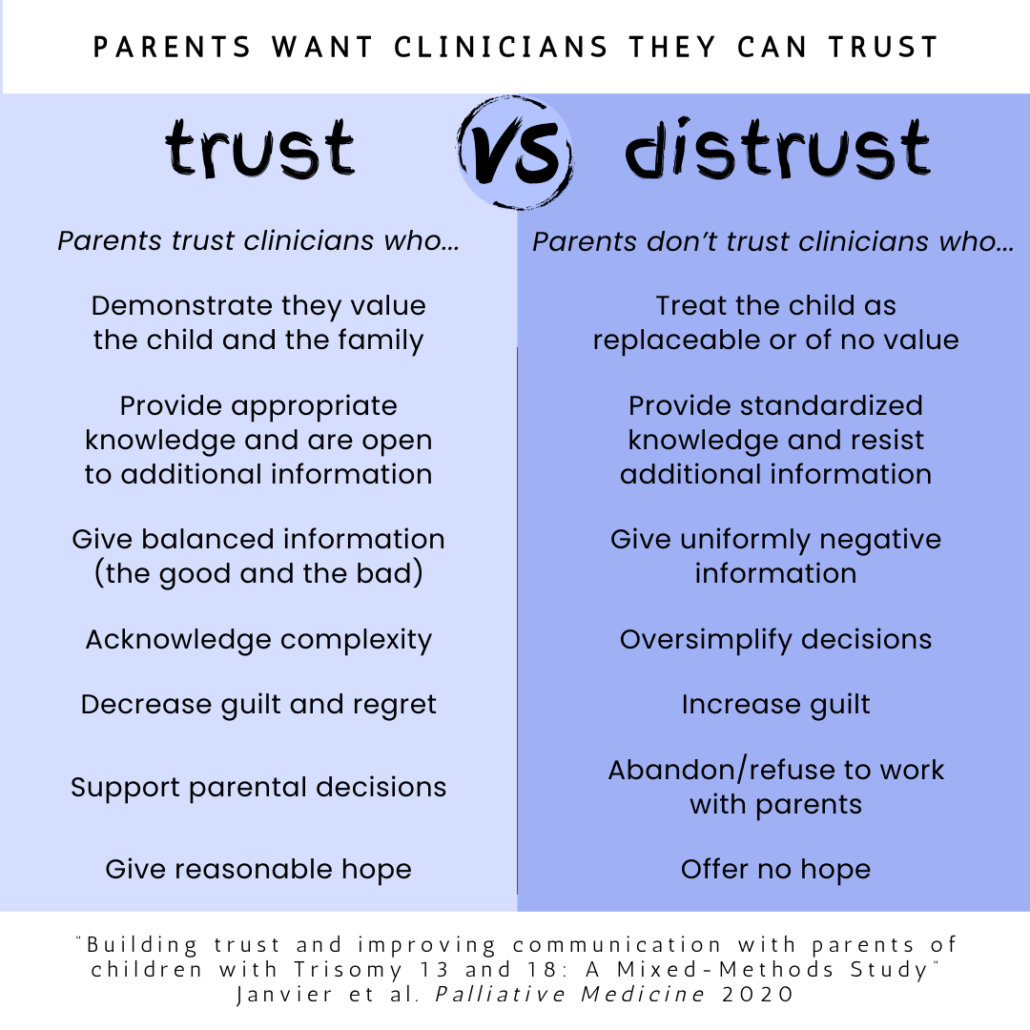
Parents trusted clinicians when they felt the clinicians
- Had appropriate knowledge,
- Cared for and valued their child and family, and
- Supported parental decision-making and presented reasonable hope.
1: Appropriate Knowledge
Parents appreciated clinicians who provided general knowledge of their child’s condition but were humble and curious about personalized situations. Some examples:
Humility and curiosity
She told me she was willing to learn with me.
She didn’t think Owen would breathe on his own. She gave me her thoughts but she also let me give mine. When Owen took himself off the vent, she told me that she was wrong and was inspired by Owen.”
Lack of humility
(I was showing him photos of kids living with this disease.) ‘Those photos aren’t real. No baby lives more than hours and you need to get your head around that.’
‘This disease is always incompatible with life, always. I know.’
‘I’m not interested in these articles. They give hope to parents when there is no hope.’
Parents appreciated when they received balanced information from their doctors, and did not appreciate receiving uniformly negative information.
Giving balanced information
After giving us all the negatives, he told us the positives: that these children are loved and that this experience does not only have to be negative.
She told us the good and the bad, the two sides of the medal.
Giving only negative information
‘There is nothing positive I can tell you. She will take time and love away from your other children. She will make your life difficult.’
Megan had gained 10 lbs before she saw the next geneticist. ‘She is only fooling you’ was the comment made by the geneticist. Why could she not ever say something positive?
Treating all babies with the condition the same way
Trisomy 13 and 18 are heterogenous conditions, meaning some children die within weeks even with life-saving internvetions, and others live months or years even with only comfort care. It varies. Parents were less likely to trust medical teams that failed to acknowledge the variable outcomes.
‘These are conditions that are incompatible with life. All kids die.’
She said that this never finishes well.
He said that T18s all died, the sooner, the better.
2: Valuing Child and Family
Parents appreciated medical teams who were kind and who made them feel their baby had value and that they were good parents.
Valuing the child
She was the first one to speak about a good life for Caleb rather than a good death.
My healthcare providers treated Levi as a person and a not a diagnosis.
We finally felt like our child mattered to someone besides us.
Not valuing the child
‘We won’t put a baby like that in our NICU.’
I was told rather unceremoniously he would not live more than a few days and it was wasteful to use up space and resources that could be better spent on a baby with a chance to survive.
[Read more – Parents Can Hear You]
3: Giving Support and Hope
Parents felt supported by clinicians who were there for them during difficult decisions, advocated for their children, and provided hope.
Supportive interactions
They suggested that we treat Tessa’s time in the womb as part of her life. It made her life more meaningful to our younger children and to us.
They wanted to know her name, unlike the others before birth that called her IT.
‘You can bathe her, change her, be there for her. Make sure you tell the other nurses that you know how to do it. You are great.’
They took pictures of our family.
‘You have done so well. She is lucky to have parents like you.’
Adverse interactions
I was told I need to think of my other children and the burden their disabled sibling could be on our family.
‘How could you have carried that to term?’
‘There’s one simple decision: terminate and get on with your life. It’s a no brainer.’
‘Well I guess it’s like when your dog dies, and you go buy a new dog.’
‘If you had testing earlier you could’ve done something about this! [abortion]’
From an ultrasound tech: ‘Why are you here if you are just waiting for this r*****ed baby to die?’
Giving reasonable hope
‘He said ‘time will tell.’ That allowed hope.’
‘Let’s hope for a good outcome: that he can go home with you.’
‘We’re going to do everything we can to give you time with her.’
Allowing no hope
‘We can’t tell you anything positive because that will give you hope.’
‘There is nothing we can do.’ That’s the worst thing a parent can hear.
I was told the only way I could get an appointment with the OB was if I was booking a termination.
Parents feeling abandoned
[We were] told that we’d be at the bottom of the list for any future medical intervention.
‘The things needed to help your baby are things that this hospital just isn’t willing to do.’
‘We can’t do this in our hospital. You’ll have to find somewhere else.’
In this study, of children who lived longer than 3 months, 74% of parents felt they had to fight for their child to get needed interventions, and 35% felt judged for the medical decisions they made. Some parents found doctors they trusted only after giving up on others.
I got pressure to terminate my pregnancy. They told me she would ruin my life and there was no hope. This was too much. My baby was worth it and I would get what she needed. We went somewhere else.
When parents felt that clinicians thought their child was “better off dead,” or had no value, they didn’t trust the clinicians and “conflicts often commenced.”
Parents of children with Trisomy 13 or 18 speak up
At the end of this survey, the authors list parental recommendations to clinicians working with families in these circumstances. Some of these recommendations are:
- Know the name of our child and use it.
- Know the details of “our case” (charts/tests) before communicating with us.
- Personalize the information: tell us what organs are malformed, and which are not, and how these findings may affect the possible outcomes.
- Emphasize the spectrum and uniqueness of each child and the lack of control we both have on many of these outcomes.
- Balance the information. We need to know that caring for a disabled child is challenging, that experiencing the death of our child will likely be the most difficult time in our lives. But also tell us that our child’s life-even if short-can have a positive impact on our family.
- Recognize that this is a difficult time for us, that we are doing our best. Empower us as parents by telling us what we are doing well.
- Give us reasonable hope, as appropriate. For example, hope we can spend moments with our child, that we can meet our child at birth.
- Words are important: don’t tell us our child is a waste of resources and will harm us. Tell us our child has a life-limiting condition, not a lethal condition that is incompatible with life.
- Be specific and focus on what you will do, not what you do not want to do. Don’t use suffering as a means to discourage non-futile interventions.
- Suggest parents connect with a trisomy support group, such as Support Organization for Trisomy 13/18 (SOFT): http://trisomy.org
- Remember you are important to us and our family.
Much of the above info is available in this Twitter thread as well as this video:
If you appreciate our work and would like to help, one of the most effective ways to do so is to become a monthly donor. You can also give a one time donation here or volunteer with us here.